Overview of Natural Killer T-cell Lymphoma (NKTL)
Natural Killer T-cell Lymphoma (NKTL) is an aggressive subtype of Non-Hodgkin Lymphoma. In early stages of the disease it can have a very good response to treatment and may be cured. However, more advanced stages, while they may respond well to treatment at first, often relapsed NKTL and can be harder to treat.
However, there has been a lot of research into NKTL in recent years, and new ways of treating it are being tested with new types of medications. Some of these are having good success in early trials, so even if you have an advanced stage NKTL, there is reason for hope.
What is NKTL?
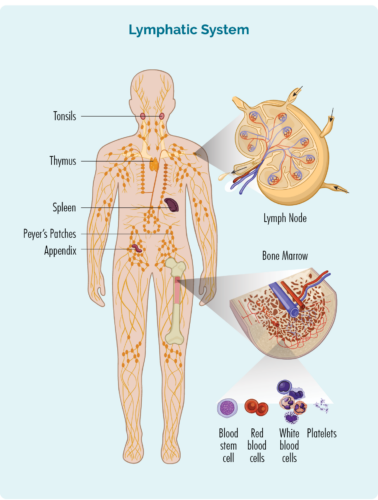
NKTL is a cancer of Natural Killer (NK) T-cells. These cells are a type of white blood cell referred to as lymphocytes. NKTL starts when changes to your genes happen resulting in your NK cells not forming properly. They can become cancerous and grow out of control, make new cancerous cells and spread throughout your body.
Understanding NK and T-cell Lymphocytes
Lymphocytes are an important part of our immune system that protect us against infection and disease, and regulate our immune system to prevent autoimmune attacks. Auto immune attacks happen when our immune system is overactive or faulty and begins to fight our own body instead of infection and disease.
About Natural Killer (NK) cells and T-cell Lymphocytes
- T-cells are made in our bone marrow, mature in our thymus, but can live in any part of our lymphatic system – including our lymph nodes.
- Most T-cells need to be activated to work effectively. They are usually resting in our thymus or other parts of our lymphatic system, and only wake up and fight infection when other immune cells let them know there is an infection or disease to fight. When they wake up, T-cells can travel to any part of our body to fight the infection or disease.
- Some T-cells are responsible for “regulating” the immune response. This means that once an infection has been destroyed, the Regulatory T-cells tell other immune cells to “stand down” so they don’t keep fighting and cause harm to our good cells.
- Natural Killer (NK) cells are often called “NK T-cells”. They are specialised immune cells that recognise and destroy germs and cancer cells. Unlike other T-cells, NK cells do not need to be activated to fight cancer. They are ready to fight at all times, and actively move around your body on the look-out for cells that have cancerous changes.
- After fighting an infection or disease, some T-cells become “Memory cells”. They remember everything there is to know about the infection and how to fight it. That way, if we ever get the same infection or disease again, our immune system can fight it a lot more quickly and effectively.
- Some T-cells help other immune cells, such as B-cell lymphocytes to work effectively. These T-cells are called “Helper T-cells”.
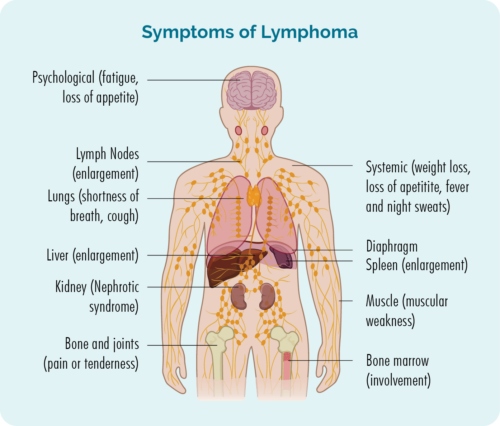
Symptoms of NKTL
When you have NKTL you may have some symptoms that are more specific to the NKTL subtype of lymphoma, or more general symptoms. Some of the symptoms more specific to NKTL include:
- ulcerations or areas of broken skin in your nose, the top part of your mouth or throat
- sores that break through your nose or other areas of your face that don’t heal
- changes to the symmetry (evenness) of your face
- difficulty breathing through your nose and/or feeling of stuffiness
- blood nose or bleeding from your mouth
- sore throat
- changes to your voice
- changes to your vision from pressure of the tumour, or weeping from your eyes
- difficulty eating or swallowing.
Diagnosis and staging of NKTL
The first step to getting a diagnosis is to have a biopsy of the area of your body affected. This may be done during surgical procedure under a general anaesthetic or you may only need a local anaesthetic, depending on the area to be biopsied. If you also have swollen lymph nodes, you will have a biopsy of the lymph node too.
You may need different types of tests to get diagnosed with T-cell lymphoma, work out your subtype, stage and grade. Watch the video below to hear from Consultant Haematologist Dr Dejan Radeski about what tests you may need.
Why do some people develop NKTL?
In many cases we don’t know why lymphoma in some people and not in others. Many risk factors have been identified as increasing your risk of getting certain lymphomas, but many people with those same risk factors do not develop lymphoma.
Epstein Barr Virus
We do know that people with Natural Killer T-cell Lymphoma (NKTL) have markers of a virus called Epstein Barr Virus (EBV) on their tumour cells. EBV is the virus that causes glandular fever – also called mono, or the kissing the disease. The virus is known to change the way some of our lymphocytes work and is thought to contribute to the development of NKTL.
EBV is a very common virus, and most people have it before they reach adulthood and the damage to some lymphocytes can last a very long time. However, it is important to know that most people that have had EBV do not develop lymphoma.
Cytogenetics

Cytogenetic tests are done to check for genetic variances that may be involved in your disease. The tests used to check for any genetic mutations are called cytogenetic tests. These tests look to see if you have any changes in chromosomes and genes.
We usually have 23 pairs of chromosomes, and they are numbered according to their size. If you have NKTL, your chromosomes may look a little different.
What are genes and chromosomes
Each cell that makes up our body has a nucleus, and inside the nucleus are the 23 pairs of chromosomes. Each chromosome is made from long strands of DNA (deoxyribonucleic acid) that contain our genes. Our genes provide the code (recipe) needed to make all the cells and proteins in our body, and tells them how to look or act. Each strand of DNA has many different genes.
Cytogenetic changes in NKTL
Some of the changes found in some people with NKTL include what is called a deletion. A deletion is when a part of the chromosome is missing and so you do not have the gene needed to tell your damaged cells to repair or destroy themselves. This means that the damaged cells continue to grow, become cancerous and then make new cancerous cells.
A common deletion in NKTL is when a part of the bottom section of the chromosome number 6 is missing. This can be written as del(6q 21-25). The “q” describes the bottom part of the chromosome while the 21-25 describes the exact location on the DNA where the genes are missing.
Proteins
There are other cytogenetic changes that can be involved in your lymphoma. Some changes may result in different proteins growing on your lymphoma cells – such as PD-L1 , CD30 or CD38 that have been found on the tumour cells of some people with NKTL. These proteins are the target of medications called immune checkpoint inhibitors or monoclonal antibodies, that are used to destroy your lymphoma cells.
It is important to know what type of proteins are found on your lymphoma cells, because some treatments called monoclonal antibodies work only on lymphomas with these proteins.
Mutations
Mutations are changes to your genes that affect how they work and can stop them from recognising and destroying lymphoma cells. Some common mutations found on NKTL cells include:
- TP53
- DDX3X
- STAT2
- JAK3
- MGA
- BCOR
- ECST
- MCL1.
Understanding these mutations helps researchers develop new treatments that specifically target these mutations and give you more treatment options.
Ask your Doctor
Ask your doctor about your individual changes and how these changes affect your treatment options. If you have any of the above mutations or changes, ask your doctor what medications are available that target these changes.
Also ask if there are any clinical trials you are eligible for that may target some of the cytogenetic changes in your lymphoma cells. Not all clinical trials are available at every hospital or state. If you are willing to travel to be part of a trial, let your doctor know how far you are willing to travel. In some cases there may even be international trials you may be eligible for.
Treatments for Natural Killer T-cell Lymphoma
Once all the results from your biopsy and staging scans have been completed, your doctor will review them to decide the best possible treatment options for you. They may even meet with other specialists in a multidisciplinary meeting to make sure all your needs are covered.
Some things they will consider when deciding the best treatment options to offer you include:
- the stage of lymphoma you have
- any symptoms you’re getting
- how the lymphoma is affecting your body
- your age
- any other medical conditions you have, medications you’re taking, and your over health and wellbeing
- your own preferences once you have all the information.
Consulting with other Haematologists
Because NKTL is so rare, your haematologist may also consult with other hematologists to discuss your case and the best treatment for you. This happens at a multidisciplinary team meeting involving haematologists, radiologists, pathologists, radiation oncologists, nurses. MDT are mainly local (within the hospital or district) but national MDTs are available through the Australasian Lymphoma Alliance (ALA) T-cell Alliance.
Chemotherapy is a term used to describe many different medications that destroy fast-growing cells. Because they destroy fast-growing cells they are effective at treating many types of cancer, including Natural Killer T-cell Lymphoma.
Common Side-effects
Chemotherapy medications cannot tell the difference between healthy and cancerous cells. They only see that they are fast-growing. This means some of your good healthy cells can also be attacked by chemotherapy resulting in unwanted side effects such as:
- mouth sores
- nausea and vomiting
- diarrhea or constipation
- hair loss
- dry skin
- a drop in healthy blood cells
- fatigue – extreme tiredness not improved with rest or sleep.
Healthy cells are able to repair and reproduce more healthy cells quicker than cancerous cells, so you will have chemotherapy in “cycles”. You will have a round of chemotherapy, then a break while your healthy cells recover, and then another cycle. How many cycles you have and the break in between will depend on the treatment you get and your individual circumstances.
Chemotherapy protocols for NKTL
Some of the common chemotherapy protocols used to treat NKTL include:
- SMILE – Steroid [dexamethasome] Methotexate, Ifosphamide, L-asparaginase, Etoposide. You will also have supportive medications to help prevent side -effects and complications. These will include:
- calcium folinate to prevent toxicity from methotrexate
- mesna to protect your bladder from the ifosphamide
- GCSF to help your white blood cells recover.
Monoclonal antibodies (MABs) are medications that engage your immune system to help it fight the lymphoma more effectively.
There are different types of MABs and they work by sticking to a protein on your lymphoma cell. The MAB then sets off signals that alert your immune system to the threat of a lymphoma cell so your immune system can mount an attack and destroy the lymphoma.
In some cases, lymphoma cells can have a protein on them (PD-L1) that tricks your immune system into thinking it is a healthy cell. When the MAB attaches to these proteins it strips the lymphoma cell of its “mask” so your immune system can see it as a lymphoma cell. These MABs are called immune checkpoint inhibitors.
Other MABs are made with a medication toxic to lymphoma cells attached to them. They then seek out the protein (such as CD30 or CD38) on the lymphoma cell and stick to it. By sticking to lymphoma cell, these MABs deliver the toxic medication straight into the lymphoma cell to destroy it. These MABs are called conjugated MABs.
Some monoclonal antibodies that may be used to treat NKTL include:
- pembrolizumab, nivolumab (immune checkpoint inhibitor)
- brentuximab vedotin (conjugated MAB)

Radiotherapy uses high-energy x-rays (radiation), to kill cancer cells. It can be used as a treatment on its own, or with other treatments such as chemotherapy.
The X-rays cause damage to the cell’s DNA (the genetic material of the cell) which makes it impossible for the lymphoma to repair itself. This causes the cell to die. It usually takes a few days or even weeks after radiation treatment begins for the cells to die. This affect can last for several months though, so even months after you finish treatment, the cancerous lymphoma cells can still be destroyed.
If your NKTL is diagnosed in the early stages of disease, this may be the only treatment you need. However, it is also often given along with chemotherapy.
A stem cell transplant is a procedure that may be used to treat your lymphoma, or to keep you in remission for longer if there is high chance your lymphoma will relapse. Your doctor may also recommend a stem cell transplant for you when your lymphoma relapses.
A stem cell transplant is a complicated and invasive procedure that occurs in stages. Patients undergoing a stem cell transplant are first prepared with chemotherapy alone or in combination with radiotherapy. The chemotherapy treatment used in stem cell transplants is given at higher doses than usual. The choice of chemotherapy given in this stage depends on the type and intent of the transplant.
More information on Stem Cell Transplants
For more information on stem cell transplants see our following webpages.
Stem cell transplants – an overview
Autologous stem cell transplants – using your own stem cells
Allogeneic stem cell transplants – using somebody else’s (a donor’s) stem cells
Clinical trials are an important way of finding new and better ways to treat lymphoma. We always recommend asking your doctor about any clinical trials you may be eligible. Especially when you have a rare cancer such as NKTL, it offers extra opportunities to try different treatments that would otherwise not be available to you.
There are no guarantees with clinical trials, as their purpose is to test new medications or combinations of treatments to see if they work better than the current treatments.
Talk to you doctor about clinical trials if you are interested in participating in one.
Second-line and other treatments
Many people have a good response from first-line treatment and will go into remission. This is where there is no detectable sign of lymphoma left in your body. But it is common for the NKTL to come back after a time in remission, this is called a relapse.
In some cases, your NKTL may not improve with the first-line treatment. If this happens, your NKTL is said to be refractory (or not responding) to treatment.
If you have refractory NKTL or have relapsed, you will need to start a different treatment. This next treatment is called second-line treatment.
Second-line treatments will depend on the type of treatment you had in the past, and if these treatments had a chemotherapy called asparaginase or not. There are many different treatments your haematologist can recommend. Some may include:
Survivorship, living with and after NKTL
A healthy lifestyle, or some positive lifestyle changes after treatment can be a great help to your recovery. There are many things you can do to help you live well with NKTL.
Many people find that after a cancer diagnosis, or treatment, that their goals and priorities in life change. Getting to know what your ‘new normal’ is can take time and be frustrating. Expectations of your family and friends may be different to yours. You may feel isolated, fatigued or any number of different emotions that can change each day.
Goals after treatment
The main goals after treatment for your NKTL is to get back to life and:
- be as active as possible in your work, family, and other life roles.
- lessen the side effects and symptoms of the cancer and its treatment.
- identify and manage any late side effects.
- help keep you as independent as possible.
- improve your quality of life and maintain good mental health.
Cancer Rehabilitation
Different types of cancer rehabilitation may be recommended to you. This could mean any of a wide range of services such as:
- physical therapy, pain management .
- nutritional and exercise planning.
- emotional, career and financial counselling.
Summary
- Natural Killer T-cell Lymphoma (NKTL) is a subtype of Peripheral T-cell Lymphoma which starts when T-cells outside of your lymph nodes become cancerous.
- It often starts in your face, most commonly your nose or the area behind your nose.
- There are many symptoms you can experience – some are general to all lymphoma subtypes and some are related to the area of your lymphoma.
- NKTL is an aggressive type of lymphoma needing treatment very soon after diagnosis.
- As with most aggressive lymphomas, NKTL often responds well to treatment at first and you may go into a period of remission however, relapse is common with T-cell lymphomas so you may need treatment more than once.
- Clinical trials are a good way to try new medications you would not otherwise have access to, but there is no guarantee they would be better than other treatments.
- There is a lot of support available to you during and after treatment for NKTL. Talk to your medical team about any extra support you may need.
- You are not alone, you can call our Lymphoma Care Nurses to talk about your lymphoma, treatment or other concerns related to your lymphoma. Click on the Contact Us button at the bottom of the screen for contact details.